Peripheral venous disease (PVD), also known as chronic venous insufficiency (CVI), is a common but often overlooked condition that affects millions of people worldwide. It occurs when the veins in the legs are unable to efficiently return blood to the heart, leading to a range of symptoms that can significantly impact an individual’s quality of life. In this blog, we will explore what PVD is, its causes, symptoms, and treatment options.,We will also showcase Dr. Achintya Sharma’s expertise,a renowned specialist in the field, who plays a pivotal role in diagnosing and managing this condition.
What is Peripheral Venous Disease?
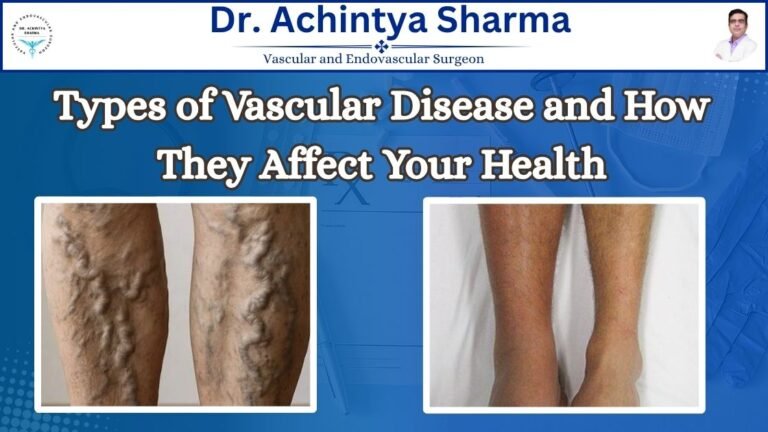
Peripheral venous disease is a condition where the veins, particularly those in the legs, fail to return blood back to the heart as efficiently as they should.This can occur when vein walls weaken or valves that regulate blood flow are damaged.Normally, valves in the veins prevent blood from flowing backward, but in people with this disease, these valves become weak or damaged, causing blood to pool in the lower extremities.
Causes of Peripheral Venous Disease
Understanding its causes can help individuals take preventive measures to avoid the development or worsening of this condition. Some of the main causes and risk factors for this disease include:
- Aging: As people age, the veins in their legs become less elastic and more prone to damage.
- Genetics: A family history of varicose veins or other vein-related conditions increases the likelihood of developing PVD.
- Obesity: Excess weight puts additional pressure on the veins in the legs, which can weaken the valves over time.
- Prolonged Standing or Sitting: Standing or sitting, common in office workers and healthcare professionals, increases the risk of developing PVD.
- Pregnancy: Pregnancy hormones and increased blood volume pressure leg veins, often causing venous insufficiency.
- History of Deep Vein Thrombosis (DVT): Previous blood clots can damage the veins and lead to chronic venous insufficiency.
- Hormonal Changes: Hormonal fluctuations, especially those occurring during pregnancy, menopause, or due to hormone replacement therapy (HRT), can weaken the vein walls.
Symptoms of Peripheral Venous Disease
PVD symptoms can differ based on how severe the condition is.Some common symptoms include:

- Swelling: Swelling in the lower legs, especially after long standing or sitting, is one of the most noticeable signs.
- Aching: Many individuals experience a dull, throbbing aching in the legs, which can worsen after standing for long periods.
- Varicose Veins: Enlarged, twisted veins that are visible on the surface of the skin are a common sign of PVD.
- Cramping: Muscle cramps, particularly at night, are often associated with venous insufficiency.
- Skin discoloration: Over time, PVD can cause skin discoloration, dryness, or the development of ulcers on the legs or ankles.
- Itching or Heaviness: Individuals may feel a sense of heaviness or tightness in their legs, along with itching or irritation of the skin.
- If these symptoms sound familiar, it may be time to consult a specialist like Dr. Achintya Sharma, who can assess your condition and recommend a suitable treatment plan.
Treatment Options for Peripheral Venous Disease
If you or someone you know is experiencing symptoms below, seeking medical attention is crucial. The earlier it is diagnosed, the more effective the treatment options will be. There are several treatment approaches for managing this disease, including lifestyle changes, medical therapies, and, in more severe cases, surgical interventions.

1.Lifestyle Modifications:
- Exercise: Regular physical activity, such as walking or swimming, can improve circulation and strengthen the muscles in the legs.
- Weight Management: Maintaining a healthy weight helps reduce the pressure on the veins and can prevent the progression of PVD.
- Elevating the Legs: Raising the legs periodically helps reduce swelling and improves venous return to the heart.
- Avoid Prolonged Standing or Sitting: Taking breaks to move and stretch can prevent blood from pooling in the legs.
2.Compression Therapy: Wearing compression stockings or bandages can help improve blood flow in the legs and reduce symptoms of swelling and pain. These stockings gently squeeze the lower legs to help blood flow upward.
3.Medications: In some cases, doctors may recommend medications to help manage the symptoms of PVD. These may include pain relievers, anti-inflammatory drugs, or medications that improve circulation.
4.Sclerotherapy: This minimally invasive procedure involves injecting a solution into varicose veins to close them off, redirecting blood flow to healthier veins.
5.Endovenous Laser Therapy (EVLT): EVLT uses laser energy to close off damaged veins, reducing symptoms and preventing further complications.
6.Vein Stripping and Ligation: In more severe cases, surgical removal or closure of damaged veins may be necessary. This is usually done with local or general anesthesia.
For expert advice and personalized care for PVD, consult Dr. AchintyaSharma, with his extensive experience in vascular medicine, can provide you with the best possible patient care tailored to your unique needs.
Prevention and Maintaining Healthy Veins
- Prevention plays a key role in managing peripheral venous disease. You cannot control age or genetics, but you can take proactive steps to reduce the risk:
Stay Active: Regular exercise, especially activities that engage the leg muscles, helps keep the veins healthy and prevents blood from pooling. - Avoid Tight Clothing: Wearing tight clothes, especially around your waist and legs, can limit blood flow and lead to vein problems.
- Maintain a Healthy Weight: Reducing excess weight helps alleviate pressure on the veins and minimizes the risk of PVD.
- Leg Elevation: Make a habit of elevating your legs while resting to promote blood flow and reduce swelling.
- Seek Medical Advice: If you notice swelling, pain, or varicose veins, consult Dr. Achintya Sharma or a professional. Early diagnosis and intervention can help prevent complications.
Conclusion
Peripheral venous disease is a common but serious condition that can impact your quality of life. It is essential to understand the symptoms, causes, and treatment options available to manage this condition effectively. By adopting lifestyle changes, seeking medical attention when necessary, and utilizing the expertise of specialists like Dr. Achintya Sharma, you can take control of your health and reduce the impact of PVD on your life. Don’t let venous insufficiency go untreated early intervention is key to maintaining healthy veins and improving your overall well-being.