Vascular illness is a silent but dangerous health issue affecting millions worldwide. It refers to disorders that affect the blood vessels—arteries and veins—and can lead to life-threatening complications if left unmanaged. One of the most significant risk factors is diabetes, a chronic condition that affects how your body processes blood sugar. This blog explores how diabetes and vascular illness are interconnected and why timely management is critical.
Understanding Vascular Illness
Vascular illness includes a range of conditions such as peripheral artery disease (PAD), atherosclerosis, and varicose veins. These conditions occur when blood vessels are damaged, narrowed, or blocked, impeding normal blood flow. Reduced circulation not only affects the extremities but also increases the risk of stroke, heart attack, and even amputation in severe cases.
Diabetes and Its Role in Vascular Complications
Diabetes, particularly when poorly controlled, damages the inner lining of blood vessels over time. High blood sugar levels cause inflammation and accelerate the build-up of fatty deposits in arteries—a condition known as atherosclerosis. This can restrict blood flow and heighten the chances of developing vascular illnesses.
Key Stats for 2025:
- According to the International Diabetes Federation, over 640 million people globally are expected to have diabetes by 2030.
- Diabetics are 2 to 4 times more likely to develop cardiovascular or vascular complications compared to non-diabetics.
- In India alone, 1 in 3 diabetic patients is at risk of developing peripheral artery disease.
How Diabetes Affects Blood Vessels
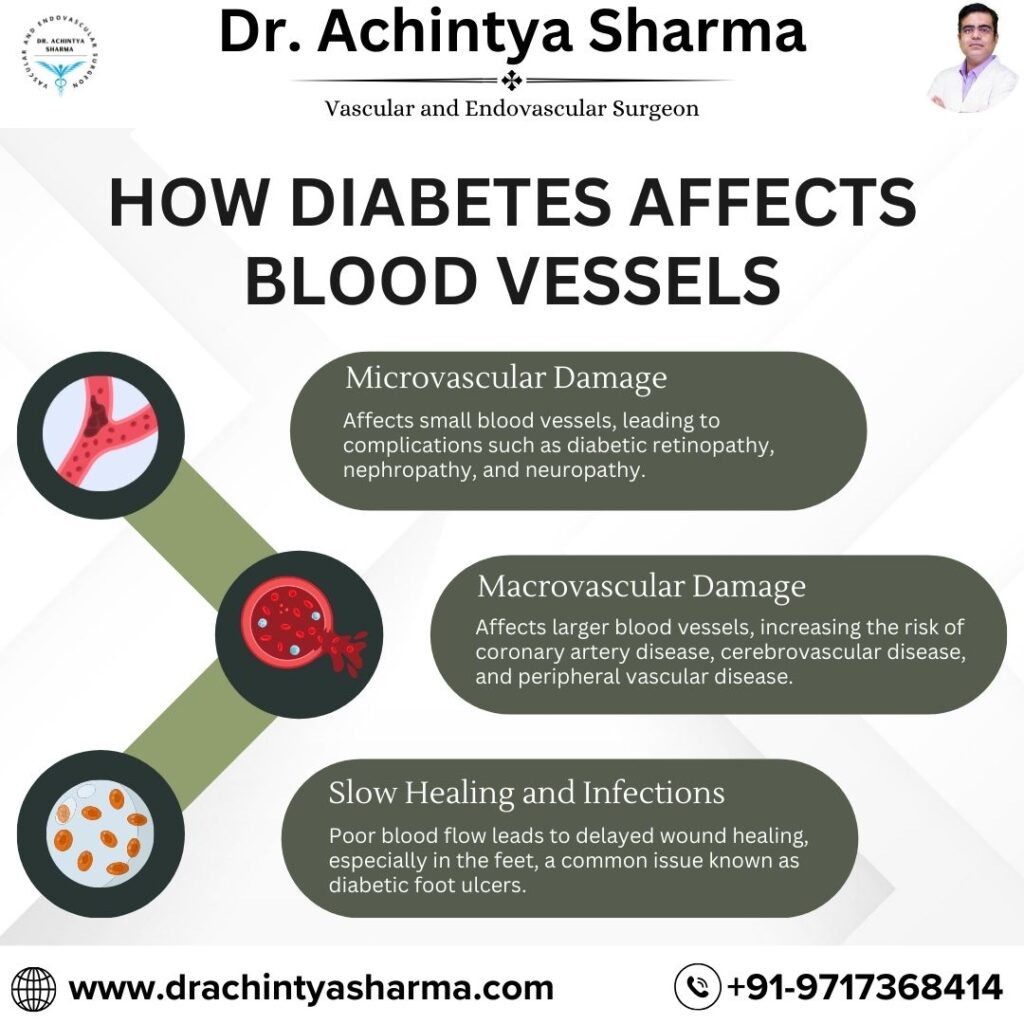
- Microvascular Damage
Affects small blood vessels, leading to complications such as diabetic retinopathy, nephropathy, and neuropathy. - Macrovascular Damage
Affects larger blood vessels, increasing the risk of coronary artery disease, cerebrovascular disease, and peripheral vascular disease. - Slow Healing and Infections
Poor blood flow leads to delayed wound healing, especially in the feet, a common issue known as diabetic foot ulcers, which can progress to gangrene if untreated.
Common Symptoms to Watch Out
If you have diabetes, watch out for these early signs:
- Leg pain while walking (claudication)
- Numbness or weakness in limbs
- Cold feet or hands
- Non-healing sores or wounds
- Swelling in the legs or ankles
Recent Advances in Diagnosis and Treatment
Diagnostic Tools:
- Ankle-Brachial Index (ABI): Compares blood pressure in the ankle and arm to detect PAD.
- Doppler Ultrasound: Visualizes blood flow through vessels.
- Angiography: Identifies blockages in blood vessels.
Treatment Options:
- Lifestyle Modifications: Strict blood sugar control, quitting smoking, and regular exercise.
- Medications: Blood thinners, cholesterol-lowering drugs, and medications for blood sugar control.
- Minimally Invasive Procedures: Angioplasty and stent placement.
- Surgical Options: Bypass surgery for severe cases.
Preventive Measures for Diabetics
Managing diabetes effectively is the best defense against vascular illness. Here are some preventive tips:
- Monitor your blood sugar levels regularly.
- Maintain a healthy diet rich in fiber and low in saturated fats.
- Exercise at least 30 minutes a day, five times a week.
- Schedule regular check-ups with your vascular specialist.
Final Thoughts
Vascular illness is one of the most serious complications associated with diabetes, but it’s also one of the most preventable. Recognizing the early signs and understanding the link between these two conditions can help you make informed decisions about your health. With early intervention and proper care, many vascular complications can be delayed or even avoided.
Dr. Achintya Sharma offers comprehensive vascular assessments and state-of-the-art treatments to help patients manage both diabetes and vascular conditions effectively. Whether it’s preventive care or advanced surgical intervention, our team is committed to restoring healthy circulation and improving quality of life.
Frequently Asked Questions (FAQs)
1. How does diabetes cause vascular illness?
Diabetes leads to high blood sugar levels, which can damage the inner lining of blood vessels over time. This damage restricts blood flow, increasing the risk of peripheral artery disease (PAD).
2. What are the early signs of vascular illness in diabetics?
Common early signs include leg pain while walking, cold or numb extremities, slow-healing wounds (especially on the feet), and changes in skin color or texture.
3. Can vascular illness be reversed if caught early?
While it may not be fully reversible, early detection and proper treatment can significantly slow down its progression and reduce complications.
4. What tests are done to detect vascular illness?
Doctors may recommend tests like the Ankle-Brachial Index (ABI), Doppler ultrasound, CT angiography, or blood flow studies to diagnose vascular issues.
5. Are diabetics more prone to amputations due to vascular illness?
Yes. Poor blood circulation and nerve damage can lead to non-healing ulcers and infections, increasing the risk of amputations, especially in the feet.
6. How can I reduce my risk of vascular illness if I have diabetes?
Managing blood sugar levels, maintaining a healthy lifestyle, avoiding smoking, exercising regularly, and having routine vascular screenings are key to lowering the risk.