Venous thrombosis is a serious medical condition that occurs when a blood clot forms in a vein. In most cases, this trouble silently builds up inside the deeper veins of our legs — people call this sneaky condition deep vein thrombosis, or simply DVT.If ignored, the condition can become life threatening – like a clot reaching the lungs, which is called pulmonary embolism. Understanding the causes, symptoms, risk factors, and treatment options is crucial for early diagnosis and effective management of venous thrombosis.
What is Venous Thrombosis?
When blood starts to gather and harden inside a vein, it leads to a condition known as venous thrombosis — a silent troublemaker that can turn into a major health threat if ignored. It typically occurs in the deep veins of the legs or pelvis, but it can also affect other areas of the body. These clots behave like unexpected roadblocks inside your blood highways, cutting off the smooth traffic and causing pain, swelling, and sometimes serious damage. When a clot breaks loose and travels to the lungs, it can result in a pulmonary embolism, which is a medical emergency.
Causes of Venous Thrombosis
Doppler ultrasound is a test method that is as accurate in finding clots hidden inside veins as searching with a flashlight in the dark.
There are several reasons why a blood clot might form in a vein. The most common causes include:
When you stay still for too long — like being glued to your seat or lying in bed for days — your blood flow slows down, giving clots the perfect chance to quietly settle in.
Injury to the vein: Surgery or accidents can damage veins and lead to clot formation.
Medical conditions: Certain conditions, like cancer or autoimmune disorders, can increase clotting risk.
Inherited disorders: Some people are born with genetic mutations that make their blood more likely to clot.
Medications: Hormone therapy or birth control pills can raise the risk, especially in women who smoke.
Symptoms of Venous Thrombosis
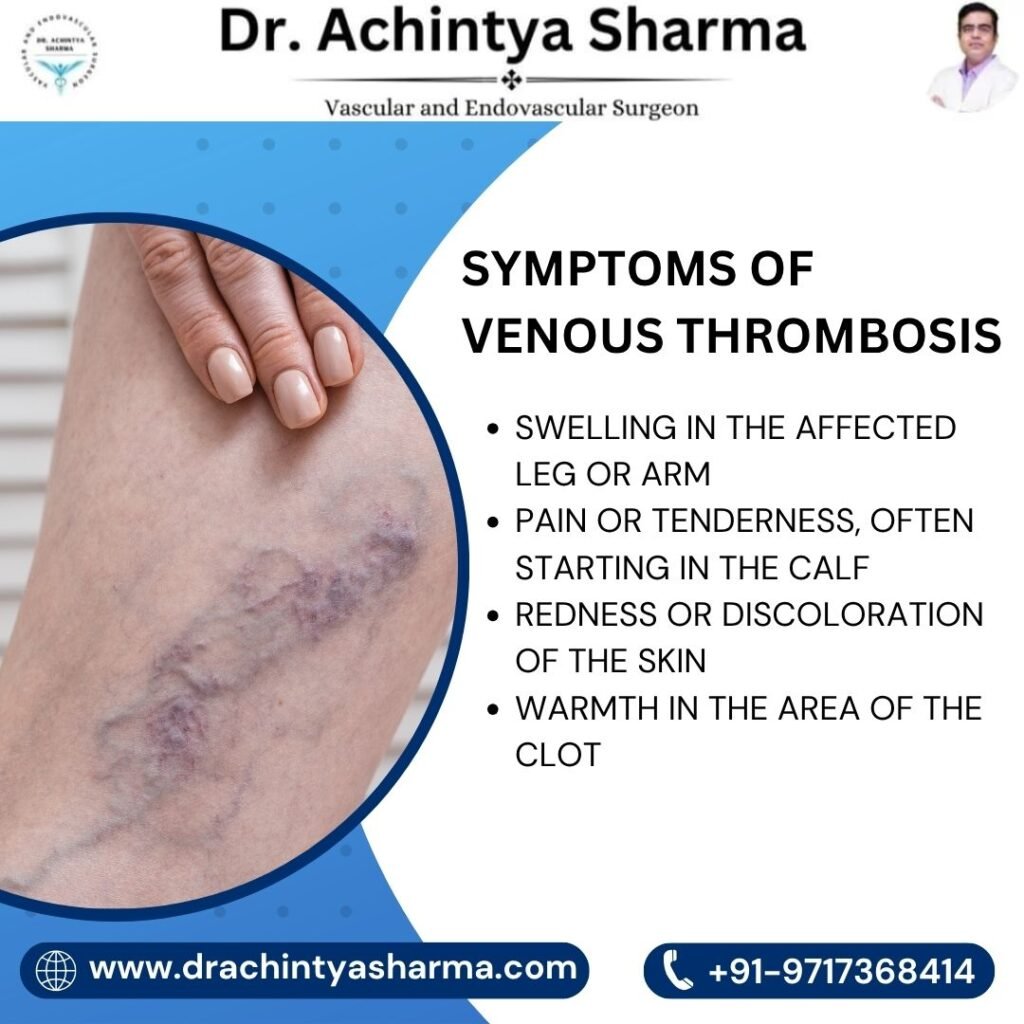
Venous thrombosis doesn’t knock with the same sound every time — its signs shift based on where the clot is sitting and how much trouble it’s causing inside.Common signs include:
- Swelling in the affected leg or arm
- Pain or tenderness, often starting in the calf
- Redness or discoloration of the skin
- Warmth in the area of the clot
- In cases of pulmonary embolism, symptoms can include chest pain, shortness of breath, rapid heartbeat, or coughing up blood
It’s important to seek medical attention if you experience any of these symptoms, especially after surgery or long travel.
Risk Factors
Plenty of things, some we notice and some we miss, quietly add layers to your risk of getting venous thrombosis over time:
- Age: Risk increases after age 60
- Obesity
- Smoking
- Pregnancy and postpartum period
- Cancer and chemotherapy
- Long hospital stays or recent surgeries
- Family history of blood clots
Understanding these risk factors can help you take preventive steps to lower your chances of developing venous thrombosis.
Diagnosis
Doctors typically use imaging tests to confirm a diagnosis of venous thrombosis. These include:
- Doppler ultrasound is a test like removing the enemy hidden inside the veins without detecting them – the most reliable way to identify clots hidden in deep veins.
- D-dimer blood test: Measures substances released when a clot breaks down
- Venography is like switching on neon lights inside your veins — a special dye lights up the hidden paths and shows where the blockage is playing hide and seek
- CT or MRI scans: Helpful in detecting clots in the pelvis or lungs
- Early diagnosis can significantly reduce the risk of serious complications.
Treatment Options
Treating a clot isn’t just about making it vanish — it’s about freezing its growth, blocking any new ones from forming, and most critically, ensuring it never takes a dangerous trip to the lungs where it could turn deadly. Common treatments include:
Anticoagulants (blood thinners): These medications prevent clots from getting larger. Common examples include warfarin, heparin, and newer drugs like apixaban.
Thrombolytics: These are clot-busting drugs used in severe cases.
Think of compression stockings: like silent traffic controllers for your legs — they guide stuck blood to move freely, ease the swelling, and restore calm in the bloodstream chaos.
Surgical procedures: In rare cases, a filter may be placed in the inferior vena cava (IVC) to stop clots from reaching the lungs.
Prevention of Venous Thrombosis
Preventing venous thrombosis involves lifestyle changes and medical strategies, especially for those at high risk:
Stay active: Regular exercise improves blood flow.
Avoid long periods of sitting: Get up and walk around during long travel or workdays.
Stay hydrated: Dehydration can make your blood thicker.
Compression stocking:Wear compression stockings if prescribed.
Follow doctor’s advice after surgery, including taking prescribed medications.
When to See a Doctor
If you notice symptoms like sudden swelling, pain, or skin discoloration, especially after a flight, surgery, or long period of inactivity, consult a doctor immediately. Early intervention can prevent dangerous outcomes.
Conclusion
Venous thrombosis is an often overlooked but potentially life-threatening condition. It may develop quietly, but with awareness, timely detection, and proper medical attention, it can be managed and prevented. Know the risks, recognize the symptoms early, and don’t hesitate to consult experts like Dr. Achintya Sharma if you’re concerned. Whether you’ve been immobile for long periods, recently had surgery, or lead a sedentary lifestyle, your attentiveness can protect your health. Don’t wait for danger signs to escalate. Act promptly. Stay aware. Stay safe.