Diabetes presents challenges far beyond glucose monitoring, including diabetic foot issues—a critical yet frequently overlooked threat. Impacting millions globally, diabetic foot problems can rapidly progress to painful ulcers, infections, and even amputations if ignored. The encouraging news? Simple daily habits and timely medical care can dramatically reduce these risks and preserve your mobility.
This comprehensive post dives into diabetic foot essentials: what causes them, key early warning signs to watch for, and practical, actionable prevention strategies. You’ll gain expert perspectives from Dr Achintya Sharma, a renowned specialist in diabetes management, dedicated to helping patients protect their feet and maintain optimal health.
Defining Diabetic Foot Issues
Describes various foot-related troubles stemming from prolonged diabetes. Consistently high sugar levels harm nerves—an issue known as neuropathy—and impair circulation to the lower limbs through peripheral artery problems. This duo heightens chances of cuts turning into ulcers, infections, or worse outcomes like amputations.
Far from minor aches, these problems involve reduced sensitivity, slow-healing injuries, and elevated infection risks. Studies show nearly one in four diabetics faces a foot ulcer sometime. Grasping these risks empowers better diabetes management.
Root Causes of Diabetic Foot Trouble
Two primary factors drive diabetic foot development:
- Nerve Impairment (Neuropathy):
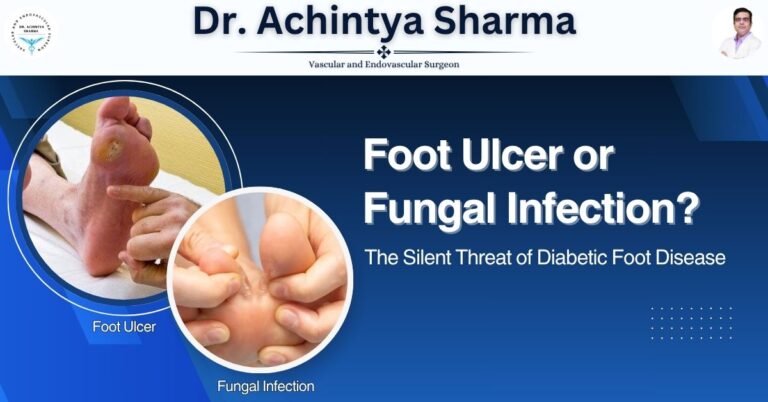
Excess glucose gradually destroys foot and leg nerves, causing pins-and-needles feelings, numbness, or total loss of sensation. Minor injuries like scrapes or rubs go unnoticed, festering into bigger problems. - Circulatory Challenges:
Diabetes hardens and narrows vessels, starving feet of vital blood supply. Without adequate nutrients and oxygen, small wounds linger, inviting bacteria.
Combined, these create a perfect storm for persistent ulcers and severe infections.
Key Warning Signs to Spot Early
Catching issues promptly can preserve mobility. Stay alert for:
- Tingling or loss of feeling in toes/feet
- Sudden sharp pains or heat sensations
- Skin discoloration or unusual foot arches
- Hard, cracked skin patches
- Non-healing cuts or fluid-filled spots
- Localized swelling, heat, or inflammation
- Unusual smells from skin breaks
Spot any? Seek medical advice fast—procrastination risks major setbacks.
Practical Steps to Avoid Foot Complications

Smart prevention beats reactive fixes, particularly for diabetes-related foot care. Follow these daily strategies, endorsed by pros like Dr Achintya Sharma:
1. Daily Foot Checks
Build a routine: scan soles, heels, and toes for bruises, inflammation, or thick skin. A hand mirror works wonders, or enlist a loved one’s eyes.
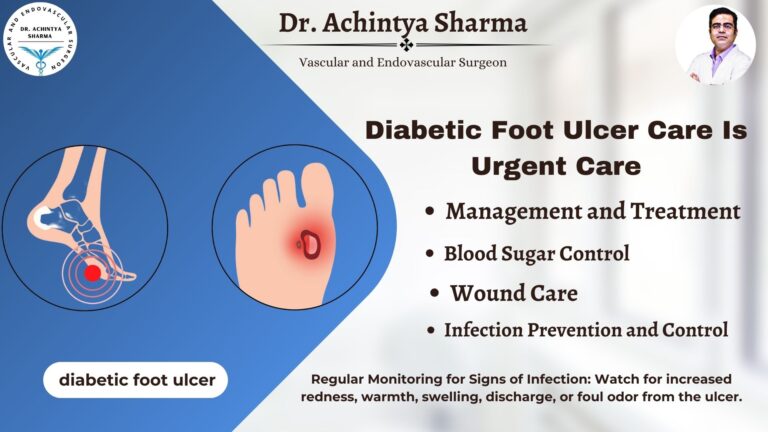
2. Steady Glucose Control
Consistent levels protect nerves and vessels. Stick to prescribed meds, balanced meals, and movement plans from your healthcare team.
3. Smart Shoe Choice
Ditch bare feet at all times. Opt for cushioned, roomy shoes and moisture-wicking socks. Skip pointy toes or anything restrictive.
4. Clean Thoroughly
Use tepid water and gentle cleanser daily, patting dry meticulously—focus on toe gaps. Hydrate dry areas sans toe crevices to dodge fungal growth.
5. No DIY Fixes
Leave corn trimming or chemical treatments to experts. Home hacks often worsen matters.
6. Regular Checkups
Annual full exams are standard; high-risk folks need them quarterly.
The Value of Specialized Guidance
Tackling diabetes foot risks solo is tough. Skilled intervention averts emergencies. Dr Achintya stresses custom strategies matching individual profiles.
His deep expertise in hormone disorders and sugar control equips patients to spot threats, track changes, and build lasting foot protection habits.
New to diabetes or long-term? Expert check-ins transform outcomes.
FAQ: Common Diabetic Foot Queries
Q1: Is diabetic foot fully reversible?
Nerve losses may persist, but prompt action halts worsening and aids recovery. Wounds respond well to targeted therapies.
Q2: What’s the ideal check-up frequency?
Annually for most, every few months if neuropathy or flow issues exist.
Q3: Do custom shoes exist for this?
Indeed—specialised pairs minimise rubbing and bolster structure, ideal for altered sensations or shapes.
Q4: Does activity reduce risks?
Yes, it boosts flow and sugar stability. Post-workout foot checks and supportive gear are key.
Q5: Best specialist for these concerns?
Your main doctor first, then hormone or foot experts like Dr Achintya Sharma for advanced handling.
Conclusion
Managing diabetic foot problems requires awareness, timely action, and consistent care. When blood sugar remains uncontrolled, even small cuts or blisters can turn into serious complications. Regular foot checks, proper footwear, and early treatment play a crucial role in preventing infections and long-term damage. Understanding the risks empowers people with diabetes to protect their mobility and overall health. For anyone noticing swelling, pain, or slow-healing wounds, seeking expert guidance is essential. Specialists like Dr Achintya Sharma provide advanced care and help patients avoid severe complications. With the right attention, diabetic foot issues can be effectively managed.