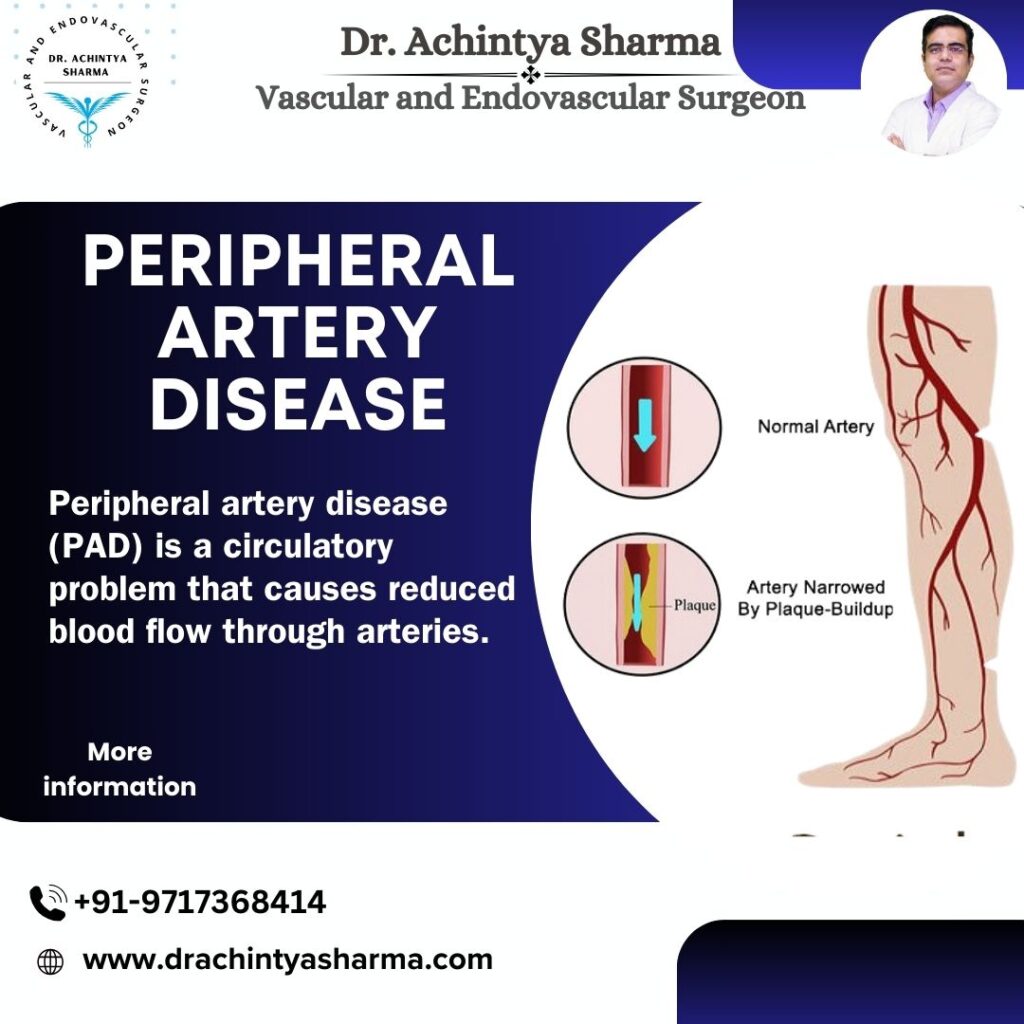
peripheral artery disease (PAD) poses a quiet yet significant danger to vascular well-being. Impacting millions globally and potentially causing a spectrum of symptoms. Ranging from intermittent claudication to more severe manifestations complications such as critical limb ischemia. This condition often goes unnoticed in its early stages, earning it the moniker of a “silent” disease. However, its implications for circulatory health are significant. Understanding its causes, symptoms, diagnosis, and treatment is crucial for preventing complications and improving overall well-being.
Atherosclerosis is primarily attributed to by this disease. Where the arteries accumulate plaque made up of cholesterol, fatty deposits, and other substances. As a result, the affected arteries become restricted, impeding the normal blood flow. peripheral artery disease is a serious condition that, if left untreated, can lead to significant health complications. Begin an enlightening exploration with us as we delve into the intricacies of this condition. Empowering you to make informed choices regarding the identification and management of PAD. Let’s start with the basics.
Causes and Risk Factors of PAD:
The chief cause of Peripheral artery disease is atherosclerosis, a systemic condition affecting blood vessels throughout the body. Several risk factors contribute to the development of PAD:
- Smoking: Tobacco smoke contains harmful chemicals that damage blood vessels and promote the build-up of arterial plaque.
- Diabetes: Individuals with diabetes have an increased risk of developing atherosclerosis. PAD due to elevated blood sugar levels affecting blood vessel integrity.
- High Blood Pressure: Hypertension contributes to the hardening and narrowing of arteries, escalating the risk of PAD.
- High Cholesterol: Elevated levels of cholesterol in the bloodstream can lead to the formation of arterial plaques.
- Age and Gender: Peripheral artery disease becomes more prevalent with age, and men are generally more susceptible than women.
- Family History: Genetic factors may predispose individuals to PAD, especially if there is a family history of vascular diseases.
Symptoms:
PAD often progresses without noticeable symptoms in its early stages. As the condition progresses, individuals might encounter the following:
- Intermittent Claudication: Pain, cramping, or leg fatigue during physical activity, such as walking, which typically subsides with rest.
- Pain at Rest: Advanced PAD may cause persistent pain or discomfort in the legs, even during periods of inactivity.
- Coolness and Discoloration: The affected limbs may feel cool, and the skin may exhibit a bluish or pale discoloration.
- Weak Pulse: A weakened or absent pulse in the affected limb may be indicative of compromised blood flow.
Diagnosis:
Prompt diagnosis of PAD is crucial for effective management. Medical professionals may utilize a variety of diagnostic instruments, including:
- Ankle-Brachial Index (ABI): This simple, non-invasive test compares the blood pressure in the ankles to that in the arms. Providing insight into the severity of PAD.
- Doppler Ultrasound: This imaging technique uses sound waves to assess blood flow and identify artery blockages or narrowing.
- Angiography: Contrast dye and X-rays are used to obtain detailed images of blood vessels. Helping visualize the extent of arterial narrowing.
- MRI or CT Angiography: These advanced imaging methods offer comprehensive views of blood vessels, aiding in diagnosis and treatment planning.
Treatment:
PAD management involves a multi-faceted approach, addressing both symptoms and underlying risk factors. Treatment options include:
- Lifestyle Modifications: Quitting smoking, adopting a heart-healthy diet, and engaging in regular exercise can improve blood flow. Overall cardiovascular health.
- Medications: Antiplatelet agents, cholesterol-lowering drugs, and medications to control blood pressure. Prescribed may be to manage underlying conditions and reduce the risk of complications.
- Angioplasty and Stenting: In cases of significant arterial blockages, angioplasty may be performed to widen the narrowed artery. Often accompanied by the placement of a stent to maintain vessel patency.
- Bypass Surgery: For severe cases, bypass surgery may be recommended to create alternative routes for blood flow around blocked arteries.
Conclusion
Peripheral Artery Disease demands attention and proactive management to mitigate its impact on vascular health. Early detection, lifestyle modifications, and medical interventions are pivotal in preventing complications. Enhancing the overall well-being of individuals affected by PAD. By understanding the causes, recognizing symptoms, and adopting a comprehensive approach to treatment. Individuals can take control of their vascular health and maintain an active, fulfilling life. Regular medical check-ups and a commitment to a heart-healthy lifestyle are crucial components of PAD management and prevention.